This Week in Sex: Advances in Infertility, HIV Prevention, and Treatment for Gonorrhea
This week, a novel approach to infertility is announced, a new vaginal ring might be able to protect from HIV transmission, and the answer to preventing drug-resistant gonorrhea may be in our own immune systems.
This Week in Sex is a weekly summary of news and research related to sexual behavior, sexuality education, contraception, STIs, and more.
New Infertility Treatment Removes Ovaries to Harvest Not-Yet-Matured Eggs
Researchers in Japan announced on Monday that a new method to help women suffering from one form of infertility has resulted in one healthy baby boy and another pregnancy. The women suffered from a condition known as primary ovarian insufficiency in which the ovaries prematurely stop releasing eggs. About one percent of women of reproductive age suffer from this condition, they are often thrown into early menopause and cannot become pregnant. Because they are no longer producing mature eggs of their own, their only option for infertility treatments has been to use a donor egg.
This new experimental procedure seems a bit like science fiction: doctors remove ovaries from the woman, cut them into small cubes, treat the cubes with egg-stimulating drugs, treat the woman with similar drugs, and then put the cubes back into the woman’s abdomen to wait for the eggs to mature.
To picture this, it helps to remember that ovaries are about the size and shape of a large Greek olive. Inside, they have thousands of microscopic little chambers called follicles. Each follicle holds an unmatured egg (or oocyte). A woman is born with all the eggs she will ever have but they are suspended in this immature state. In a working ovary, one of these oocytes typically matures every other month (the two ovaries usually take turns) leading to ovulation and then either pregnancy or menstruation.
Of the 27 women who underwent this new treatment for the study in Japan, five produced mature eggs. Like in other in vitro procedures, a woman’s eggs were then fertilized with her partner’s sperm and the resulting embryo (if one developed) was transplanted into her uterus.
The study’s author, Dr. Kazuhiro Kawamura, told the press, “I always felt emotional anxiety [about the treatment approach] … but when I saw the healthy baby, my anxiety turned to delight. The couple and I hugged each other in tears.”
It will likely be years before this procedure is widely available.
New Vaginal Ring May Prevent HIV Infection
A study in the Proceedings of the National Academy of Sciences has shown that a new vaginal ring developed by researchers at Northwestern University in Illinois may be able to protect women from HIV transmission. The ring is actually a polymer tube filled with the powdered form of the antiretroviral drug Tenofovir. It is designed to be worn continuously for 30 days. When the ring gets moist, which would happen naturally during most acts of intercourse, the polymer expands and some of the drug is released into the vagina.
Tenofovir is a nucleoside reverse transcriptase inhibitor (NRTI), which works to reduce the amount of HIV in a person’s blood. Studies have found that oral Tenofovir can also dramatically reduce a person’s risk of acquiring HIV. In 2012, the Food and Drug Administration approved the use of a combination drug containing Tenofovir. As part of a prevention method known as PrEP (pre-exposure prophylaxis), the drug can be taken once a day by adult men who do not have HIV but are at high risk because of their sexual behavior or intravenous drug use.
Though Tenofovir is usually taken orally, the researchers who invented the vaginal ring, which is known as TDF-IVR, believe that by delivering the drug topically right to where it is needed, they can use a lower dosage. Moreover, women would not have to remember to take a pill each day, nor would they have to remember to insert a ring right before intercourse. Public health experts have been wanting a prevention method that women across the world can use without necessarily having to inform a partner who would object.
The researcher recently tested TDF-IVR in non-human primates and found that it was able to block 100 percent of the simian version of HIV. Human trials will likely start next month.
Currently, there are also trials taking place to see if a gel form of Tenofovir can prevent HIV transmission when applied rectally prior to anal sex.
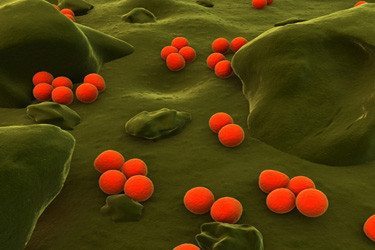
Researchers Boost Immune Systems to Fight Gonorrhea Reinfection
As Rewire reported, the Centers for Disease Control and Prevention (CDC) recently named antibiotic-resistant gonorrhea an urgent threat, noting that almost 30 percent of the current 800,000 cases that occur each year are resistant to one or more of the drugs used to treat the infection. One reason that the bacteria that causes gonorrhea has been so resilient and adaptable is the high rates of reinfection among individuals. New research, published in the Journal of Infectious Diseases, suggests that the answer to preventing reinfection and ultimately antibiotic-resistance may be boosting the immune system’s response to the bacteria.
Michael Russell, a microbiologist at the State University of New York, Buffalo has been studying gonorrhea for 20 years. In a press release, he explains his belief that the bacteria that cause gonorrhea is able to re-infect individuals easily because it alters a person’s immune system and prevents them from developing long-term resistance to the bacteria the way they would to other germs.
Our immune systems generally have two responses to illness: the innate or immediate response that lets us fight off a current infection and the adaptive response that develops antibodies to help better fight later infections. Russell found that people with gonorrhea infections had a high rate of a chemical in the body known as IL-10 and believes that this suppresses the adaptive response. He and a colleague then devised a way to use a different chemical, IL-12, to counteract IL-10.
So far, the treatment has only been used in laboratory mice (who were first infected with gonorrhea) but it has been very effective. Those mice who were given IL-12 responded better to antibiotics and were less likely to get re-infected when re-exposed than the control group of mice. Russell believes that IL-12 prevents the immune system from being “tricked” into suppressing its own adaptive immune response.
As the CDC notes, the best way to hold back the tide of antibiotic resistant gonorrhea is to prevent gonorrhea infections in the first place. Preventing re-infections, obviously, is also important.
